The Ethics of BCIs for Autism
Brain-Computer Interfaces can change us. When should they?

The singularity is a thorny proposition. Like a collapsing building, it leaves few options—its grace is that we are aware of it; we might see it coming. Scenarios involving the singularity yawn like black holes in my daydreams: is there a way around it, this existential hammer?
Elon Musk thinks the answer is brain-computer interfaces: more specifically, linking ourselves to AI before it becomes superhuman. This is ostensibly why he’s helming NeuraLink.
I’ve always loosely agreed with this, but it feels like a necessary evil: the smallest, most manageable ethical disaster we can pick from. Even if BCIs simplify our dilemma, from the singularity to the ethical development and distribution of super-human intellect—that’s still a hard problem, no?
In a class on biomedical ethics, I learned that my professor (the inestimable Gary Comstock) was an expert on the ethics of brain-computer interfaces. The BCI/Singularity dilemma was the first question I asked him, in a half-hour conversation after class. It was a discussion we continued throughout the semester, culminating (in a sense) in my final paper. That’s what I’m adapting here.
I’m going to start with a narrow scope—the ethics of therapeutic BCIs as applied to autism—and tie it back to Singularity concerns at the end.
Some of the ideas here are summarized cogently in Barnbaum’s The Ethics of Autism, a book I can’t recommend enough. You can get it from Amazon.
Table of Contents
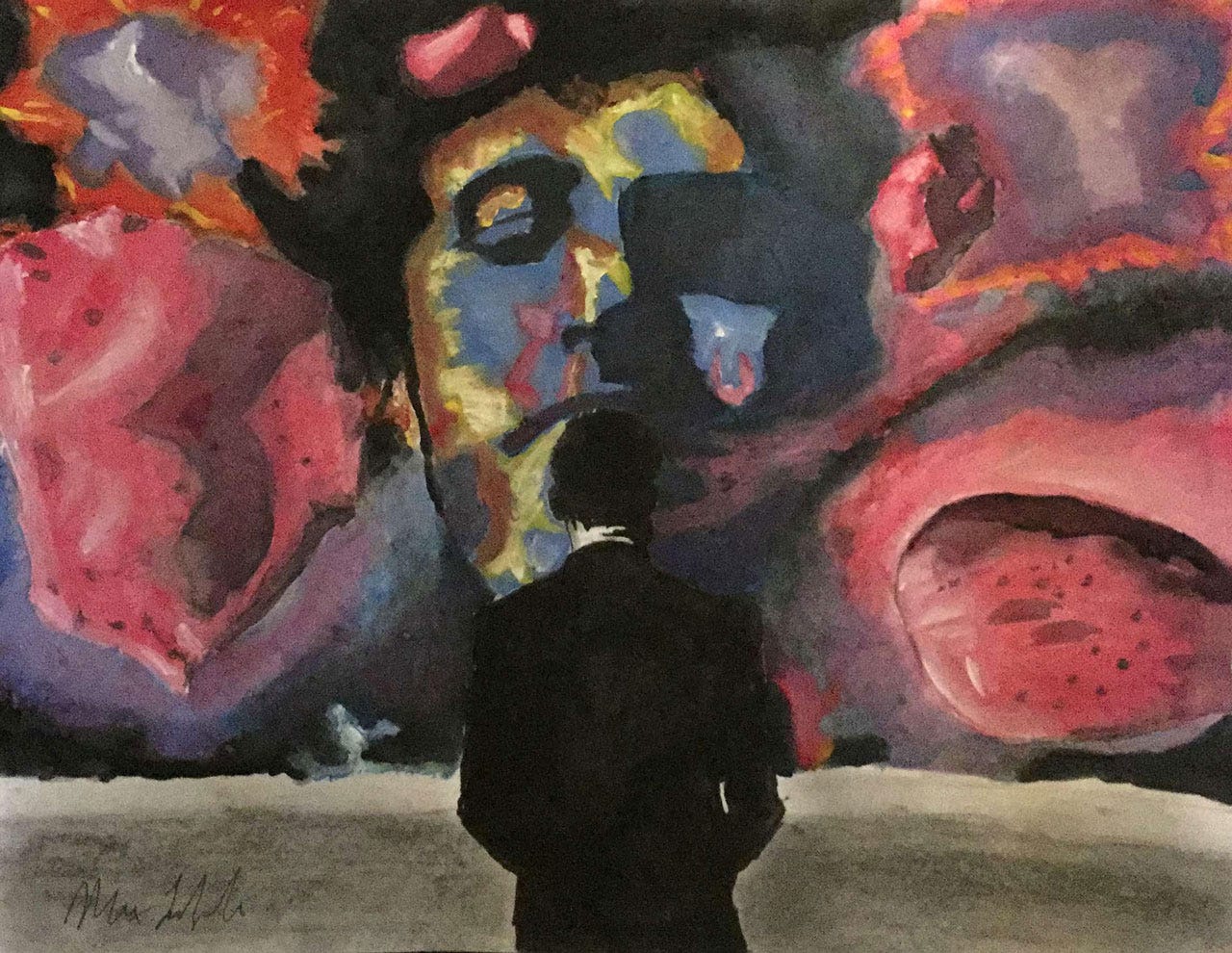
Ethics is hard, so this will take a while. I’ve scattered throughout some of my favorite works by Max LaZebnik, a 25-year-old artist with autism, because they’re fascinating, and I’d like to keep at center-stage the precept that those with autism can be as vibrant, compelling, and human as the rest of us. You can (and should) check out the rest of his work on Surrebral, his site.
Ethical Pros and Cons of BCI Use
Autism and Mental Solipsism
Diversity versus Disease
Autonomy and Consent
Identity and Humanity
Theory of Mind
Patterned Behaviors
Benefits of Autistic cognition
Risks to Brain-Computer Identity
Augmentation and the Ship of Theseus
Therapy, Enhancement, and the Singularity
Closing
Understanding our brains has long proved an elusive challenge—many fundamental insights didn’t emerge until the early twentieth century, and they didn’t begin to coalesce into the interdisciplinary field of cognitive science until the 1940’s (see, e.g., the CalTech’s Hixon Symposium, featuring some of the greats—von Neumann, McCulloch, Lashley).
A century later, a maturing understanding of the brain—alongside drastic advancements in computing—has enabled the creation of advanced interfaces between brains and computers.
Ethical Pros and Cons of BCI Use
These interfaces (BCIs) hold vast potential, for such simple therapeutic applications as restoring lost motor function to more advanced enhancements of human cognition (which I’ve covered before). I will restrict my focus here to therapeutic BCIs: those treating disabilities, rather than enhancing natural abilities. Some of this post’s high-level ethical overview comes from the excellent review by Burwell, et al (linked next paragraph).
Ethical arguments in support of therapeutic BCIs include the restoration of autonomy and quality of life to disabled patients. But BCIs also come with a variety of objections, some of the most prominent being: that they pose significant risks to patient humanity/identity and autonomy; that their risks are, generally, unquantifiable and unjustifiable; and that their distribution will necessarily exacerbate social inequality.
Going forward, I will attempt to argue the ethical case for therapeutic BCIs in the specific, controversial context of the autism spectrum disorder.
Autism and Mental Solipsism
The past decade has observed a significant maturation in the understanding of autism as a spectrum disorder. As autism’s conception in the DSM solidified from five distinct diagnoses in 2000 to a single spectrum disorder with multiple “levels” in 2013, the number of diagnoses in U.S. 8-year-olds increased from 1 in 150 to 1 in 69.
There are two pillars of autism symptoms: deficient or absent social skills, and restricted or repetitive patterns of behavior. Autism is also characterized by an impaired or simply absent “theory of mind”, the ability to understand the desires and beliefs of others—sometimes considered a prerequisite for human metacognition.
Barnbaum’s book spends a lot of time on autism’s mental solipsism, and illustrates that the theory of mind can be missing—and so cause disability—even in patients who are otherwise high-functioning. As an example, she cites someone with autism who found herself more perturbed by an unwanted rearrangement of furniture than she was by the death of her father.
Diversity versus Disease
Debates over the ethics of autism treatment have at their foundation an ongoing debate about the nature of autism itself—more pointedly, whether or not autism qualifies as a disease.
Some cite the neurodiversity of those with autism as evidence against deserving the classification; rebuttals cite the difficulties it can cause, including an inability to form emotional connections and even the inculcation of self-harming behaviors.
Writing as an editor of the AMA Journal of Ethics, Kathleen Miller derives from the literature that (emphasis added) “there are two truths here. First, autism can be devastating; and second, autism is not a disease.” Recently the debate has grown more intricate, with the emergence of advocacy groups targeted both at curing autism the disease (Cure Autism Now, Defeat Autism Now) and celebrating autism the developmental difference (Aspies for Freedom). Here, as elsewhere in my argument, there is a salient distinction to be made between high-functioning patients with autism and those who are, in contrast, highly impaired.
Autonomy and Consent
Suppose, for a moment, a BCI appears that reliably treats autism: it restores a theory of mind, shores up social capabilities, and removes any deleterious behavioral patterns. When should autistic patients be treated with this BCI?
Advocates for autistic rights might answer, when they ask for it, and only then. This line of reasoning, intuitive on its face, assumes that autism is a form of neurological diversity, not a disease—or, at least, moreso the former than the latter—and that it does not impair the autonomy or competency of those experiencing it.
This may be true for those closer to one end of the autistic spectrum: patients with Level 1 autism, for example, may not require substantial support to overcome their social difficulties; as the categorically highest-functioning among those with autism, they would likely be judged competent in an informed decision to opt out of BCI treatment. (Would the term “patient” even apply?)
However, this is not necessarily the case for those more significantly impaired by autism. Patients with Level 3 autism are clearly not competent: they cannot handle the regular responsibilities of life without support (due to cognitive, not physical, constraints). How, then, can we expect them to make an informed decision about their own care, especially under the influence of the very disability they are meant to consider?
If a “high-functioning” patient with autism is able to make a rational, informed value judgement about the impact of autism on their life—weighing, perhaps, increased productivity against reduced social connection—then we cannot and should not attempt to make the decision for her. But we should feel obligated to make the decision for the “low-functioning” patient who clearly cannot make it for herself, and suffers because of it.
Identity and Humanity
Advocates for autism as neurodiversity might bristle at the very idea of using a BCI to treat autism: after all, wouldn’t this rob the patient of her identity, transforming her form one person—the autistic one—to another entirely?
Let’s return to our ideal BCI, which only treats autism—what is it doing? It is restoring a theory of mind, perhaps, or attenuating repetitive patterns of behavior. The question becomes: do either of these symptoms of autism constitute a significant piece of one’s identity? Let’s consider them separately.
Theory of Mind
The theory of mind is considered a basic human-cognitive faculty. An autistic patient who regains that theory of mind has obviously changed; but it would be reductive to claim merely that she has lost her identity. Rather, it can be argued that she has restored a missing piece of it.
Often, an absent or impaired theory of mind results in an inability to form emotional connections, something which can also be achieved by certain drugs. If someone lived their entire life under the emotion-blunting influence of such drugs, would it be considered a damage to their identity to relieve them of those symptoms?
I argue this would be more akin to a restoration of their natural identity, in the same way that curing a patient’s congenital lower-body paralysis constitutes a restoration of their physical self.
Caveat: the above implies a notion of disability as harmful error from the natural, which is itself subject to significant debate. Some in the Deaf community argue that disabilities are determined socially, not biologically; however, this argument is less persuasive for autism (page through the DSM).
The neurodiversity advocate for autism might instead object: who are we to administer therapy on the basis of neural norms, which may shift in the future? (See, for example, this.)
One might object that a disabled person’s identity is partly formed by their experience of reality, which would change without the presence of the disability. But curing someone who has already lived with the disease would not change that piece of their identity: it has already formed. To adopt, briefly, a computational model of mind, the difference is between modifying someone’s memory and correcting their processor.
Patterned Behavior
Repetitive patterns of behavior are subtler, in that they can contribute to or overwhelm an identity, depending on their intensity and frequency. This is clear at extremes: self-harming behaviors, or rituals that distract from all else, damage or obfuscate other components of a patient’s identity. In contrast, patterned behavior that manifests itself as mere intense interest fits more cleanly into a comprehensive picture of identity.
As autonomy depends on the level of one’s neuroses, so too does identity. Whereas, for autonomy, a threshold must be set where a patient’s symptoms overwhelm their ability to make rational decisions, we might here recommend the attenuation or removal of repetitive behaviors when they exert an undue influence on other aspects of identity. For example: attention to detail is a significant component of one’s identity; but if it cannot be had without crippling emotional capacity, there is more identity to be gained without than with it.
A similar criteria for removal of “disabling” neurological phenomena might be a consequentialist analysis of their impact on quality of life—in effect, how truly disabling they are. We might consider the benefits and detriments conferred by Level 1 autism to be, if nothing else, an acceptable trade-off (and, indeed, many with Level 1 autism do); but few would make a similar judgement for Level 3 autism. This, like any analysis of a spectrum disorder, becomes a matter of degrees.
I experienced this personally with OCD, another spectrum disorder that often accompanies autism: as a child, my anxiety was so debilitating as to render me almost non-functional. Now, with appropriate treatment, it persists, but only in concert with innumerable other cognitive processes that collectively define me. It renders positive and negative effects that are, in net, small enough to make for a difficult therapeutic calculus.
This is not a perfect analogy: the rigid procedures of OCD are patently upsetting (if sometimes productive), whereas autism’s obsessions might be enjoyable; furthermore, OCD does not feature autism’s lack of a theory of mind. Nevertheless, I believe the salient detail persists: that the just because a disease is a part of one’s identity, does not mean one would not benefit from mitigating it.
Benefits of Autistic Cognition
What of other facets of autistic cognition, especially those considered to be positive? Those with autism often exhibit an enhanced capacity for focus and attention to detail (see this, this). It is possible an autism-therapy BCI might revert these positives to something more ordinary; in such cases, the choice to make this identity trade-off should be made by a rational, competent patient—or, if the patient is too impaired to be competent, by their physician, in concert with family.
Risks to Brain-Computer Identity
Beyond the intentional changes there is the risk of off-target / unintended modulations of brain activity in non-ideal BCIs. Human cognition manifests itself in a yet-untangled web of neurological interactions; an interface ignorant of these subtleties may unduly influence them. However, scientific precedent suggests these risks will diminish over time, as BCI interfaces grow more sophisticated and higher-resolution, and as advancements in neuroscience further contextualize the activity being modulated.
It is worth noting also that, in a sense, we already engage in activities which modulate our neural activity in detrimental and unquantified ways. For example, many consider use of the internet to be a meaningful and useful activity; however, the advent of social media has had demonstrably profound but simultaneously poorly-understood effects on our behavior and sense of self. A well-made BCI, if significantly more direct / lower-latency in its modulation of brain activity, would arguably be far more precise in its effects, while offering fewer risks to identity.
Augmentation and the Ship of Theseus
It’s easy to imagine a point where BCI-induced modulation of brain activity clearly crosses from corrective to something more aggressive: a BCI that simply stopped all brain activity, for example, would clearly nullify its subject’s identity. So would one that flooded neurons with noise, or one that randomly attenuated certain regions of activity. But what about a BCI that intelligently modulated the activity of different neurological regions or functional modules? Would a version of me with double the linguistic capacity still be me?
Changes to individual faculties might feel like just that: modifications that do not override the whole of one’s cognition (a version of me with better face-memory, or who can solve differential equations more readily, or even with a higher IQ, is but a small step removed). But these faculties are intimately related in ways not yet well understood— the brain’s very modularity, for example, is not complete, nor is it without debate—and at some point a ship-of-Theseus concern rears its head.
To the extent that one’s identity is formed by past experiences, a version of me with all faculties boosted via BCI would, in the moment immediately after this change, still be more or less me; but thenceforth the way I experienced reality would be radically different, and the pre- and post-BCI versions of myself might diverge radically, like weather systems with similar initial conditions.
Therapy, Enhancement, and the Singularity
Such ethical dilemmas can be avoided (or, at least, dramatically delimited) by focusing only on specific therapeutic applications. Many issues in medical ethics make a key distinction between procedures for therapy and those for enhancement; typically, cases are more easily made for the former.
Therapeutic BCI’s, specifically, sidestep some of the thornier debate around humanity and equitable distribution of technology by way of their more limited scope; however, it is worth noting that the line between therapy and enhancement has been known to shift over time. Corrective cleft-palate surgery, once considered cosmetic, is now understood to be therapeutic.
In the context of BCIs, examples are more provocative. Human intelligence, as measured by IQ, has been shown to increase over time; a procedure which increased an individual’s IQ by 5 points in 1910 might be considered an enhancement, while in 2013—by which point the average had grown 30 points—that same procedure on that 1910 individual could be considered therapy.
And this, as you might have guessed, is where this all ties back into the Singularity, and makes our exploration of autistic identity more relevant.
In that more dramatic (though not infeasible) context of an eventual singularity, standard human intelligence could be considered a comparative disability, and a BCI that dramatically increases human intelligence might commensurately be viewed as a therapeutic measure. In critical contrast to autism, most average patients would be considered competent in a decision to opt into or out of it.
Closing
In this post I’ve attempted to lay out the case for the ethical use of brain-computer interfaces in treating autism. I have attempted to answer concerns on the basis of patient autonomy and identity, illustrating the role of autism’s spectrum in the process. I believe therapeutic BCIs like the ones discussed can open the door to a new regime in ethical, transformative care, restoring autonomy and identity to many patients for whom both are currently limited—and, just maybe, down the road, transforming it for everyone.